When the Centers for Medicare and Medicaid Services (CMS) published the proposed home health payment rule for 2023, it included the expected implementation of a nationwide Value-Based Purchasing (VBP) program starting in 2023.
But there was an unexpected twist.
Previously, CMS had indicated 2019 would be the “baseline” year for home health VBP, but in the proposed rule, the baseline year became 2022.
Under home health VBP, the “baseline year” establishes minimum scores required for agencies to earn either “achievement points” by exceeding the national median score from the baseline year or “improvement points” by exceeding their own score from the baseline year.
Scores are important because total performance scores from 2023 will be used to determine payment adjustments in 2025.
“The shift in baseline year left agencies in the dark about what targets they should be aiming for in 2023,” said Christine Lang, SimiTree Director of Data Analytics.
“They could track their own performance to assess what their improvement baseline score might be, but they wouldn’t have access to national 2022 numbers until mid-2023, at the earliest.”
Further complicating data assessment was the lack of updated data available on Care Compare, the official CMS website housing publicly reported health care data. CMS froze reporting during the COVID 19 pandemic, leaving in place data from 2019 instead of refreshing the data quarterly.
“This made it hard for anyone to even guess at national score trajectories in 2020,” Lang said.
Newer data available
Recently, CMS updated the data on Medicare Compare, updating metrics to represent more recent time periods.
SimiTree data analysts crunched the available numbers, looking at a period Lang calls “2021-ish,” due to a lack of uniformity among the three different types of data that will be used to determine home health VBP performance scores.
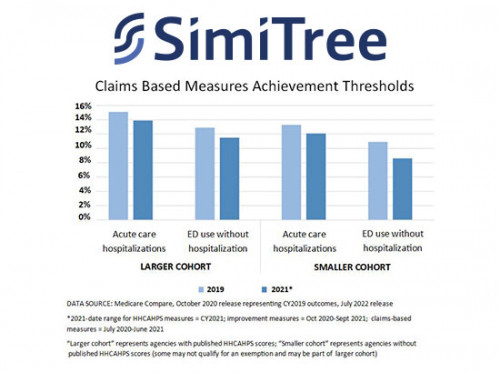
Data from CY2021 was available HHCAHPS measures; data from October 2020-September 2021 was available for improvement measures; and data from 2020-June 2021 was available for claims based measures.
“While it’s still not 2022 data, of course, and we can’t exactly replicate the larger and smaller cohort groups that CMS will divide agencies into, we can compare 2016 and 2022 numbers to shed some light on industry trends and roughly what HHAs should be expecting for 2022 standards,” Lang said.
The highlights:
- HHCAHPS patient survey scores have stayed almost identical, with only two measures seeing 2% declines
- Hospitalization and emergency care rates have dropped (improved), and smaller agencies have a higher bar to meet (with lower median scores, as lower is better for these measures)
- Improvement rates have increased, and larger agencies have a higher bar to meet
“If CMS keeps the 2022 baseline in the final rule, it means that some agencies wont earn points if they exceeded 2019 norms but don’t exceed the (what we can safely expect will be) higher 2022 scores, and most of those that outperform 2022 standards will earn fewer points than they would have with the 2019 baseline,” Lang said.
“It’s important to keep in mind, however, that 1) there are also improvement points to consider, 2) all agencies are in the same boat, and 3) at the end of the day, it’s all about how the final agency VBP scores stack up against each other,” she said. “The industry overall having lower scores will have minimal impact on the determination of which agencies experience an impact on payment or how much.”
See related article, CMS Proposes Changes to HHVBP Model