Beginning this month, home health and hospice agencies with high billing errors and denial rates could be subject to a review of between 20 and 40 claims and all supporting medical documentation for those claims under a renewed audit program.
The Centers for Medicare and Medicaid Services (CMS) resumed its Targeted Probe and Education (TPE) audits Sept. 1 after previously suspending TPE during the COVID-19 public health emergency.
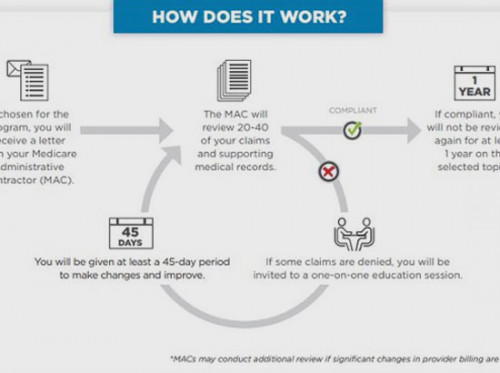
“As audits go, CMS considers TPE to be friendly, because it focuses on improvement rather than penalties,” said SimiTree Healthcare Consulting Senior manager Sheila Salisbury-Sizemore. "As part of the audit process, the provider receives one-on-one education on claims that were denied, often via a conference call, and has an opportunity to ask questions about the billing errors or oversights under review and how CMS policy applies."
“But if you are the agency being audited, of course, it may feel more intimidating than friendly,” she added.
It may also feel labor intensive and time-consuming – particularly for agencies experiencing a resurgence of COVID-19 cases.
“Responding to a TPE audit can take hours of staff resources," Sizemore said. “And with the ongoing pandemic, agencies are concerned about having the manpower to care for patients, handle worker shortages and respond to audits.”
Agencies may be able to request an extension to the usual 45-day period response time allowed to provide medical records if they can demonstrate hardship due to COVID-19.
Hardship extensions for Covid
MACs initiate TPE audits by sending a notification letter to the agency selected for audit. Between 20 and 40 claims will be examined, and agencies must provide all supporting documentation and make corrections within a 45-day period.
MACs have the discretion to grant an extension to providers who need more time to comply with the TPE medical record request due to hardship, according to Kim Skehan, Director of Compliance, Regulatory and Quality for SimiTree Healthcare Consulting.
“If an agency is unable to reply with the required timeframe due to hardship, it will be allowed to submit an extension request outlining the hardship to the MAC,” Skehan said. “This extension must be specific to restarting TPE and is intended to be temporary in nature. The ability to request an extension will coincide with the COVID-19 public health emergency.”
Who is at risk
Agencies are selected for TPE audits due to high national error rates that represent a financial risk to Medicare, according to Skehan and Sizemore.
“Frequent errors on billing claims or billing practices that CMS believes to be unusual might trigger a TPE,” Sizemore said. “Some examples of common errors that might trigger an audit include frequently submitting claims with a missing physician signature, encounter notes that don’t support eligibility for services, and missing or incomplete documentation for certification or recertification."
On its web site, Medicare administrative contractor Palmetto GBA identifies three instances in which it might initiate a TPE audit:
• Analysis of billing data indicating aberrancies or
• On targeted review and is transitioned to the TPE process based on error rate results or
• On service specific review error rate results
How we can help
If your agency is notified by letter that it has been selected for a TPE audit, the experts at SimiTree Healthcare Consulting can help. If an extension is necessary due to COVID-19, our experts can help your agency outline the nature of the hardship and submit the extension request. We can also help with the staff training needed to avoid billing errors and oversight that generate TPE audits and make certain documentation requirements are fully understood.
For more information about how we can help, call us at 800-949-0388 or contact us below.
Source: CMS